Figure 1. Covid-19 compared to other common conditions
COVID-19 typically causes fever and a dry cough. One may have aches in the body—the muscles—and if it's severe enough, there would be shortness of breath.
Gastrointestinal symptoms can occur and are an indication of more severe disease. It's not very common to have a runny nose or the sniffles, and a sore throat is not common either.
COVID isn’t just a respiratory disease; it also affects other organ systems. It can make a weak heart beat erratically, turn a manageable case of diabetes into a severe one, or weaken a frail person to the point where they fall and break something.[44]
The incubation period from exposure to onset of symptoms is between four and six days; and if you want to cover 95–98 percent of the cases it is between three and 10 days. It's pretty rare to have an incubation period outside of that range.
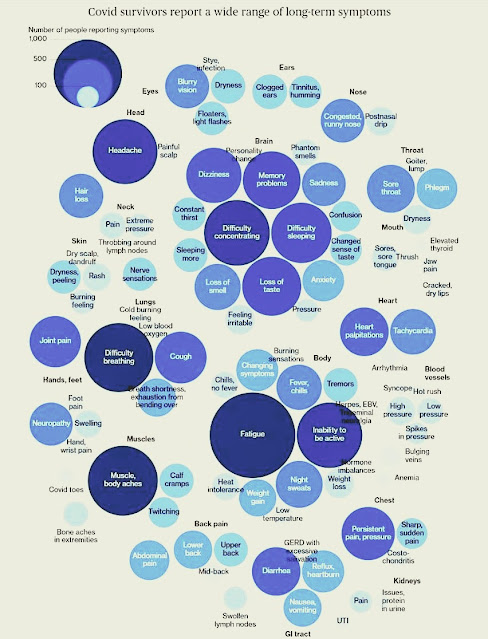
Figure 2. Covid-19 survivors report a wide range of long-term symptoms
Why COVID-19 is dangerous[1,8]
On 08/26/2021, total COVID-19 worldwide deaths were 4.47M.
SARS-CoV-2 induces an inflammatory state, evidenced by raised acute markers like interleukin-6 (IL-6), c-reactive protein (CRP), ferritin, d-dimer etc. and may lead to lung damage especially in the second week of illness owing to the cytokine storm.[43]
One of the largest studies of Covid-19 “long haulers” has proved what many doctors suspected: Not only are many patients suffering a raft of health problems six months after infection, they’re also at significantly greater risk of dying.[38]
Furthermore, Covid-19 patients who survived hospitalization were found to have a 51% increased risk of dying compared with 13,997 influenza patients who also had been hospitalized.[38]
 |
| Figure 3. Aerosols vs droplets (Sars-CoV-2 can be spread via aerosols) |
Transmissibility and Stability of Virus
What is disturbing is that virus shedding, as detected in the mouth or nose, is very, very common and could be there prior to onset of symptoms. That's why transmission could occur from asymptomatic individuals. And virus shedding could continue for days up to three weeks after a person recovers. That is extremely worrisome for the spread of this virus.
Furthermore, the stability of this virus is worrisome as well. Based on a recent study, researchers at Australia’s national science agency, CSIRO found that [22]
- At 68 ℉, COVID-19 can survive on banknotes, glass and stainless steel for up to 28 days, much longer than the flu virus which is 17 days
- However, the survival time declined as the temperature increased
- Proteins and fats in body fluids can also sharply increase virus survival times
- This helps to explain the apparent persistence and spread of SARS-CoV-2 in cool environments with high lipid or protein contamination, such as meat processing facilities
How the COVID-19 affects each individual could be different based on a person's genes,[30,31,36] pre-exiting health conditions, immunity profile history,[29] incomes, risk-taking behaviors and, also, local healthcare facilities. Read the below articles for more details:
- Even Mild Covid-19 Infections Can Make People Sick for Months
- Covid-19 survivors report a wide range of long-term symptoms (Figure 2)
- As evidence builds that COVID-19 can damage the heart, doctors are racing to understand it
- A perspective on potential antibody-dependent enhancement of SARS-CoV-2
- COVID-19 survivors suffer long term heart conditions
- Your Risk of Getting Sick From Covid-19 May Lie in Your Genes
- Male coronavirus patients with low testosterone levels are MORE likely to die from COVID-19, German hospital finds
- Covid Doctors Find a Turning Point in Life-Threatening Cases
- Strokes and mental state changes hint at how COVID-19 harms the brain
- Death Rate of Covid-19 by Age / Prior Illness / Ethnic Group
- COVID's cognitive costs? Some patients' brains may age 10 years
- The major genetic risk factor for severe COVID-19 is inherited from Neanderthals
- Neuroinvasion of SARS-CoV-2 in human and mouse brain
 |
| Figure 4. A review on mRNA vaccines at @NatRevDrugDisc (Source: [41]) |
What's the Exit Strategy
Local lockdowns and social distancing could be the emergency measure to prevent a catastrophic death toll. But no western democracy has yet been able to lay out a good plan for how normal life can resume. The Imperial College study that heavily influenced UK government policy envisions some form of social distancing until a vaccine or treatment is available. However, that could still be sometime down the road.[3]
The Hope: Population Immunity
We are looking at a world with parameters bounded by pure imagination;
where we go from here is anyone's guess.
—Will Thomson and Chip Russell
There are a few anecdotes from China about re-infection but, if you look at those reports carefully, they're not well-documented. It could be that folks just continued to shed virus from the initial infection. Only one study was formally done and it is not a human study. It's a macaque study. They infected macaques with this virus, then waited until the monkeys recovered and tried to re-infect them. They could not. That bodes well for human immunity.
We have now looked at a lot of serum from convalescent individuals and those serum samples have antibodies against the so-called spike protein of the virus. That's the protein that sits on the surface of the virus particle. By tightly binding, the antibody could neutralize the virus. Once an infected person develops antibodies, there should be protective immunity for quite some time. That's why we need to buy time for immunity to develop in the population.
What if Sars-CoV-2 mutate and quash the hope?
One aspect of Sars-CoV-2 is how it has evolved more slowly than some other viruses such as HIV or the flu. Just 40 differences have evolved so far between the most distantly related samples.[10] Although surveillance has not shown any mutations that would affect its transmissibility or virulence, scientists are watching closely in case they appear.
How about the Next 10 years Down the Road?
Based on [28], for the next 10 years, John Mauldin has predicated that:
We are going to see major advances in healthcare. I mentioned a few weeks ago the invention of Far UVC which doesn’t penetrate the skin or eyes of human beings, but will kill viruses and bacteria.
And while the pandemic has caused a major setback in worldwide poverty, I expect that to be short-lived. We will see the number living in poverty steadily decrease, as it has for the last 50 years.
References
- The Tip of the Iceberg: Virologist David Ho (BS '74) Speaks About COVID-19
- Even Mild Covid-19 Infections Can Make People Sick for Months
- [WEBCAST REPLAY] COVID-19 Pandemic Update: Analysis From Neil Howe & Daryl Jones
- Why U.S. hospitals see promise in plasma from new coronavirus patients
- Virus May Spread Twice as Fast as Earlier Thought, Study Says
- What Does Your Cough Say About Your Illness?
- The COVID-19 vaccine development landscape
- She spent 9 days in a coma and relearned how to walk. What this Covid-19 survivor wants protesters to know
- If you’re hoping a vaccine is going to be a knight in shining armor saving the day, you may be in for a disappointment. SARSCOV2 is a highly contagious virus. A vaccine will need to induce durable high level immunity, but coronaviruses often don’t induce that kind of immunity (link)
- Mutations map holds the key to bringing coronavirus under control
- Virus Likely to Keep Coming Back Each Year, Say Top Chinese Scientists (Bloomberg)
- “The virus is heat sensitive, but that’s when it’s exposed to 56 degrees Celsius for 30 minutes and the weather is never going to get that hot,” said Wang Guiqiang, head of the infectious diseases department of Peking University First Hospital. “So globally, even during the summer, the chance of cases going down significantly is small.”
- All the Covid-19 Symptoms You Didn’t Know About
- Coronavirus: Can it affect eyesight?
- What Troponin Tells Us About Myocardial Injury in COVID-19
- Clinicians then assess potential causes of troponin elevation, including hyperinflammation, which may respond to immunosuppressive therapy.
- Strokes and mental state changes hint at how COVID-19 harms the brain
- A family physician’s COVID story
- A COVID-19 vaccine: 5 things that could go wrong
- Studies detail conjunctivitis in kids, adults with COVID-19
- A perspective on potential antibody-dependent enhancement of SARS-CoV-2
- COVID-19 survivors suffer long term heart conditions
- As evidence builds that COVID-19 can damage the heart, doctors are racing to understand it
- Novel coronavirus survives 28 days on glass, currency, Australian researchers find
- CDC Expands Covid Risk Warning to Include Overweight People
- Nearly 72% of American adults are overweight (25 < BMI < 30) or obese (BMI ≥ 30)
- CDC Says Virus Can Spread Indoors in Air Beyond Six Feet
- Covid may cause sudden, permanent hearing loss – UK study
- 29-Year-Old Overcomes COVID-19, Cardiac Arrest While On Ventilator
- Hospitalised COVID-19 patients can have ongoing symptoms for months -study
- What Will Not Change
- Common cold antibodies hold clues to COVID-19 behavior
- Your Risk of Getting Sick From Covid-19 May Lie in Your Genes
- The major genetic risk factor for severe COVID-19 is inherited from Neanderthals
- 'Breakthrough finding' reveals why certain Covid-19 patients die
- Diverse and functional autoantibodies revealed in COVID-19 patients
- Diverse Functional Autoantibodies in Patients with COVID-19
- Pandemic Appears to Fuel Rise in Stress Cardiomyopathy Rates
- Genetic mechanisms of critical illness in Covid-19
- Coronavirus Deranges the Immune System in Complex and Deadly Ways
- ‘Long Hauler’ Study Shows Covid Can Kill Months After Infection
- SARS-CoV-2 uses a multipronged strategy to impede host protein synthesis
- Rapid induction of antigen-specific CD4+ T cells guides coordinated humoral and cellular immune responses to SARS-CoV-2 mRNA vaccination (good summary)
- mRNA vaccines for infectious diseases: principles, delivery and clinical translation (accessed on 08/26/2021)
- Antigenic drift: Understanding COVID-19
- Liu F. Prognostic value of interleukin-6, C-reactive protein, and procalcitonin in patients with COVID-19. J Clin Virol. 2020;127:104370.
- COVID-Hospitalization Numbers Are as Bad as They Look


No comments:
Post a Comment